Post Diploma Training in Gynecology Course Details:
Post Diploma Training in Gynecology. Mobile No: 01797-522136,01987-073965.Hotline:01969947171. Post Diploma Training in Gynecology Courses are PDT-Gynecology Course 6 Months, PDT-Gynecology Course 1 Year, PDT Gynecology Course 2 Years. 6 Months Course Fee 35,500/-, 1 Years Course Fee 70,500/-, 2 Years Course Fee 1,30,500/-.

Location of Post Diploma Training in Gynecology Course
Post Diploma Training in Gynecology. Mobile Number.01987073965.01797522136,HotLine-01969947171 HRTD Medical Institute , Abdul Ali Madbor Mention, Section-6, Block-Kha, Road-1, Plot-11, Mirpur-10 (Gol-Chattar) Metro Rail Pilar NO-249, Dhaka-1216. It is situated by the West Side of Agrani Bank, the South Side of Fire Service, Islami Bank, Janata Bank, Social Islami Bank, Medinova, Ibrahim Diabetic Hospital, the North Side of Baitul Mamur Jame Mosjid, Grave of Baitul Mamur Jame Mosjid, and East Side of Maliha Apartment.
Female Reproductive System.
Hostel Facilities in HRTD Medical Institute
Hostel & Meal Facilities
The Institute has hostel facilities for the students. Students can take a bed in the hostel.
Hostel Fee Tk 3000/- Per Month
Meal Charges Tk 3000/- Per Month. ( Approximately )
হোস্টাল ও খাবার সুবিধা
ইনস্টিটিউটে শিক্ষার্থীদের জন্য হোস্টেল সুবিধা রয়েছে। ছাত্ররা হোস্টেলে বিছানা নিতে পারে।
হোস্টেল ফি 3000/- টাকা প্রতি মাসে,
খাবারের চার্জ 3000/- টাকা প্রতি মাসে।(প্রায়)
Course Fee for Post Diploma Training in Gynecology Course 6 Months
Course Fee for Post Diploma Training in Gynecology 6 Months at HRTD Medical Institute. Admission Fee=15,500/-,Monthly Fee 3000×6=18,000/-,Exam Fee=2000, Total Course Fee=35,500/-.This Course Contains 4 Subjects .Exam Mark 400.
Course Fee for Post Diploma Training in Gynecology Course 1 Year
Course Fee for Post Diploma Training in Gynecology Course 1 Year at HRTD Medical Institute. Admission Fee=20,500/-,Monthly Fee 3500×12=42,000/-,Exam Fee=4000×2=8000, Total Course Fee=70,500/-.This Course Contains 8 Subjects .Exam Mark 800.
Course Fee for Post Diploma Training in Gynecology Course 2 Years
Course Fee for Post Diploma Training in Gynecology Course 2 Years at HRTD Medical Institute. Admission Fee=30,500/-,Monthly Fee 3500 x 24=84,000/-,Exam Fee=4000×4=16,000, Total Course. Fee=1,30,500/-.This Course Contains 16 Subjects .Exam Mark 1600.
Subjects for Post Diploma Training in Gynecology Course 6 Months
This 6 Months Course contains 4 subjects. Mobile No: 01987073965.01797522136,HotLine-01969947171
- Male Reproductive Anatomy & Physiology
- Female Reproductive Anatomy & Physiology
- Menstrual Complications & Treatment
- Gynecological Drugs & Pharmacology
Subjects for Post Diploma Training in Gynecology Course 1 Year
This 1 Year Course contains 8 subjects. Mobile No: 01987073965.01797522136,HotLine-01969947171
1st Semester
- Male Reproductive Anatomy & Physiology
- Female Reproductive Anatomy & Physiology
- Menstrual Complications & Treatment
- Gynecological Drugs & Pharmacology
2nd Semester
- Pregnancy & Lactation Care
- Gynecological Disease & Treatment
- Gynecological Surgery
- Abortion/Missccariage
Subjects for Post Diploma Training in Gynecology Course 2 Years
This 2 Year Course contains 16 subjects. Mobile No: 01987073965.01797522136,HotLine-01969947171
1st Semester
- Male Reproductive Anatomy & Physiology
- Female Reproductive Anatomy & Physiology
- Menstrual Complications & Treatment
- Gynecological Drugs & Pharmacology
2nd Semester
- Pregnancy & Lactation Care
- Gynecological Disease & Treatment
- Gynecological Surgery
- Abortion/Missccariage
3rd Semester
- Family Planning
- Menstrual Cycle & Disorders
- Pediatric and Adolescent Gynecology
- Obstetrics
4th Semester
Some Subjects Details for Post Diploma Training in Gynecology Course Given Below
Male Reproductive Anatomy & Physiology for Gynecology Course
Male Reproductive System
Definition
The male reproductive system is a group of organs responsible for production of sperm, secretion of male sex hormones (testosterone), and delivery of sperm into the female reproductive tract for fertilization.
Main Functions
- Production of sperm (male gametes)
- Secretion of testosterone
- Storage, nourishment, and transport of sperm
- Ejaculation of semen during sexual intercourse
Parts of the Male Reproductive System
1. Testes (Testicles)
- Location: Inside the scrotum
- Shape: Oval
- Function:
- Produce sperm (spermatogenesis)
- Produce testosterone
- Special feature: Temperature is 2–3°C lower than body temperature (necessary for sperm production)
2. Scrotum
- A skin pouch that holds the testes
- Function:
- Protects testes
- Regulates temperature for sperm production
3. Epididymis
- Coiled tube attached to each testis
- Function:
- Maturation and storage of sperm
- Sperm gain motility here
4. Vas Deferens (Sperm Duct)
- Long muscular tube
- Function:
- Transports sperm from epididymis to ejaculatory duct
5. Ejaculatory Duct
- Formed by union of vas deferens and seminal vesicle duct
- Function:
- Passes semen into the urethra
6. Seminal Vesicles
- Paired glands
- Function:
- Secrete fructose-rich fluid
- Provides energy and nourishment to sperm
- Contributes about 60% of semen volume
7. Prostate Gland
- Single gland below urinary bladder
- Function:
- Secretes alkaline fluid
- Increases sperm motility and neutralizes vaginal acidity
8. Bulbourethral (Cowper’s) Glands
- Small paired glands
- Function:
- Secrete mucus-like fluid
- Lubricates urethra and neutralizes acidity before ejaculation
9. Urethra
- Common passage for urine and semen
- Parts:
- Prostatic urethra
- Membranous urethra
- Penile urethra
10. Penis
- External organ
- Function:
- Delivers semen into female reproductive tract
- Also used for urination
- Contains erectile tissue
Male Reproductive Physiology for Gynecology Course
Definition
Male reproductive physiology deals with the functions and processes by which the male reproductive system produces sperm, secretes male hormones, and delivers sperm for fertilization.
Main Physiological Functions
- Spermatogenesis – formation of sperm
- Hormonal regulation – secretion of testosterone
- Maturation of sperm
- Erection
- Ejaculation
1. Spermatogenesis
Definition:
Process of formation of sperm from germ cells.
Site:
- Seminiferous tubules of testes
Duration:
- About 64–74 days
Steps:
- Spermatogonia → mitosis
- Primary spermatocytes → meiosis I
- Secondary spermatocytes → meiosis II
- Spermatids
- Spermatozoa
Requirements:
- Testosterone
- FSH
- Temperature 2–3°C lower than body temperature
2. Hormonal Control of Male Reproduction
Hypothalamic–Pituitary–Testicular Axis
- GnRH (Hypothalamus) → stimulates pituitary
- FSH → acts on Sertoli cells → sperm production
- LH → acts on Leydig cells → testosterone secretion
Testosterone Functions
- Development of male genital organs
- Secondary sexual characteristics
- Libido
- Maintenance of spermatogenesis
3. Sperm Maturation & Transport
- Sperm mature in epididymis
- Gain motility and fertilizing capacity
- Transported via vas deferens by peristaltic movement
4. Formation of Semen
Semen = Sperm + glandular secretions
| Gland | Secretion | Function |
|---|---|---|
| Seminal vesicle | Fructose | Energy |
| Prostate gland | Alkaline fluid | Motility |
| Cowper’s gland | Mucus | Lubrication |
5. Erection (Physiology)
- Controlled by parasympathetic nerves (S2–S4)
- Nitric oxide released
- Vasodilation of penile arteries
- Filling of erectile tissue with blood
6. Ejaculation
Two phases:
1. Emission
- Controlled by sympathetic nerves
- Semen enters urethra
2. Expulsion
- Rhythmic contraction of muscles
- Semen expelled out of penis
7. Sperm Characteristics
- Lifespan: 48–72 hours in female tract
- Motility essential for fertilization
- Normal count: ≥15 million/ml
Female Reproductive Anatomy for Gynecology Course
Definition
The female reproductive system consists of organs that are responsible for production of ova (eggs), secretion of female hormones, fertilization, pregnancy, and childbirth.
Functions
- Production of ova
- Secretion of estrogen and progesterone
- Reception of sperm
- Site of fertilization
- Support of fetal development
- Childbirth and lactation
Parts of the Female Reproductive System
A. Internal Genital Organs
1. Ovaries
- Paired, almond-shaped organs
- Location: Pelvic cavity, one on each side of uterus
Functions:
- Produce ova (oogenesis)
- Secrete estrogen, progesterone, relaxin
2. Fallopian Tubes (Uterine Tubes)
- Length: ~10–12 cm
- Connect ovaries to uterus
Parts:
- Infundibulum (with fimbriae)
- Ampulla – site of fertilization
- Isthmus
- Intramural part
Function:
- Transport ovum
- Site of fertilization
3. Uterus
- Hollow, muscular, pear-shaped organ
- Location: Between bladder and rectum
Parts:
- Fundus
- Body
- Cervix
Layers:
- Perimetrium (outer)
- Myometrium (muscular)
- Endometrium (inner lining)
Functions:
- Implantation
- Growth of fetus
- Menstruation
4. Cervix
- Lower narrow part of uterus
- Connects uterus to vagina
Functions:
- Produces cervical mucus
- Acts as birth canal during labor
5. Vagina
- Muscular canal (~8–10 cm)
- Connects cervix to exterior
Functions:
- Receives penis and semen
- Passage for menstrual flow
- Birth canal
B. External Genital Organs (Vulva)
1. Mons Pubis
- Fatty tissue over pubic bone
2. Labia Majora
- Outer skin folds
- Protection
3. Labia Minora
- Inner folds
- Surround vaginal and urethral openings
4. Clitoris
- Erectile tissue
- Highly sensitive
- Sexual arousal
5. Vestibule
- Area containing vaginal and urethral openings
6. Bartholin’s Glands
- Secrete mucus
- Lubricate vagina
C. Mammary Glands (Accessory Organs)
- Modified sweat glands
- Function: Milk production (lactation)
Female Reproductive Physiology for Gynecology Course
Definition
Female reproductive physiology explains the functional processes involved in oogenesis, menstrual cycle, ovulation, fertilization, pregnancy, and lactation.
Main Physiological Functions
- Oogenesis (formation of ovum)
- Hormonal regulation
- Menstrual cycle
- Ovulation
- Fertilization
- Pregnancy
- Lactation
1. Oogenesis
Definition: Formation of mature ovum from germ cells.
Site:
- Ovaries
Stages:
- Oogonia (before birth)
- Primary oocyte (arrested in prophase I)
- At puberty → meiosis resumes
- Secondary oocyte released during ovulation
- Completion of meiosis II only after fertilization
2. Hormonal Regulation (Hypothalamic–Pituitary–Ovarian Axis)
- GnRH → stimulates pituitary
- FSH → follicle development & estrogen secretion
- LH → ovulation & corpus luteum formation
- Estrogen → growth of endometrium, secondary sexual characters
- Progesterone → prepares uterus for pregnancy
3. Menstrual Cycle
Average length: 28 days (normal 21–35 days)
Phases:
A. Menstrual Phase (Day 1–5)
- Shedding of endometrium
- Caused by fall in estrogen & progesterone
B. Proliferative Phase (Day 6–14)
- Estrogen-dominant phase
- Endometrium regenerates
- Follicle matures
C. Ovulatory Phase (Day 14)
- LH surge
- Release of secondary oocyte
D. Secretory Phase (Day 15–28)
- Progesterone-dominant
- Endometrium thickens
- Prepares for implantation
4. Ovulation
- Release of ovum from ovary
- Occurs ~14 days before next menstruation
- Triggered by LH surge
- Ovum survives 24 hours
5. Fertilization
- Site: Ampulla of fallopian tube
- Fusion of sperm and ovum
- Forms zygote
- Zygote moves to uterus for implantation
6. Pregnancy Physiology
- Implantation occurs in endometrium
- hCG maintains corpus luteum
- Placenta forms → hormone production
- Gestation period: ~280 days (40 weeks)
7. Lactation
- Prolactin → milk production
- Oxytocin → milk ejection
- Occurs after childbirth
Menstrual Complications & Treatment for Gynecology Course
Definition
Menstrual complications are disorders related to the frequency, duration, amount, or pain during menstruation, usually caused by hormonal imbalance, uterine pathology, or systemic disease.
Common Menstrual Complications
1. Dysmenorrhea (Painful Menstruation)
Types
A. Primary Dysmenorrhea
- No pelvic pathology
- Caused by ↑ prostaglandins
B. Secondary Dysmenorrhea
- Due to conditions like:
- Endometriosis
- Fibroids
- Pelvic inflammatory disease (PID)
Symptoms
- Lower abdominal pain
- Back pain
- Nausea, vomiting
- Headache
Treatment
- NSAIDs (Ibuprofen, Mefenamic acid)
- Antispasmodics
- Oral contraceptive pills (OCPs)
- Heat therapy
- Regular exercise
- Treat underlying cause (for secondary type)
2. Amenorrhea (Absence of Menstruation)
Types
- Primary: No menstruation by age 15
- Secondary: Absence for ≥3 months
Causes
- Pregnancy
- Stress, weight loss
- PCOS
- Thyroid disorders
- Pituitary disorders
Treatment
- Treat underlying cause
- Hormonal therapy (estrogen/progesterone)
- Lifestyle modification
- Management of PCOS or endocrine disease
3. Menorrhagia (Heavy Menstrual Bleeding)
Features
- Excessive bleeding (>80 ml)
- Prolonged menstruation (>7 days)
Causes
- Fibroids
- Hormonal imbalance
- IUCD
- Bleeding disorders
Treatment
- Tranexamic acid
- NSAIDs
- Hormonal therapy (OCPs, progesterone)
- Iron supplementation
- Surgery (D&C, myomectomy, hysterectomy if severe)
4. Metrorrhagia
- Irregular bleeding between periods
Causes
- Hormonal imbalance
- Polyps
- Cervical or uterine pathology
Treatment
- Hormonal regulation
- Treatment of local pathology
5. Oligomenorrhea
- Infrequent menstruation (>35 days cycle)
Causes
- PCOS
- Stress
- Excessive exercise
- Thyroid disorders
Treatment
- Hormonal therapy
- Weight management
- Treat endocrine disorders
6. Polymenorrhea
- Frequent menstruation (<21 days cycle)
Causes
- Hormonal imbalance
- Pelvic infection
Treatment
- Hormonal regulation
- Treat infection
7. Premenstrual Syndrome (PMS)
Symptoms
- Mood swings
- Irritability
- Breast tenderness
- Bloating
- Fatigue
Treatment
- Lifestyle modification
- Exercise
- Low salt diet
- NSAIDs
- Oral contraceptives
- SSRIs (severe cases)
8. Premenstrual Dysphoric Disorder (PMDD)
- Severe form of PMS
- Psychological symptoms prominent
Treatment
- SSRIs
- Hormonal therapy
- Counseling
Gynecological Drugs & Pharmacology for Gynecology Course
Gynecological pharmacology involves a diverse range of drugs to manage conditions across a woman’s lifespan, including hormonal therapies, anti-infective agents, and medications for labor and delivery. The appropriate medication choice depends heavily on the patient’s age, specific condition, and reproductive goals.
Hormonal Therapies
Hormonal agents are widely used in gynecology to address menstrual disorders, menopause, endometriosis, and polycystic ovary syndrome (PCOS).
- Oral Contraceptives: These combined estrogen and progestin pills work by managing the discharge of FSH and LH, preventing ovulation. They are also used to treat menstrual irregularities and breakthrough bleeding.
- Gonadotropin-Releasing Hormone (GnRH) Analogues: Drugs like leuprolide or goserelin are used to manage conditions such as endometriosis and uterine fibroids. Continuous administration inhibits the normal function of the hypothalamus-pituitary-ovarian axis, creating a hypoestrogenic state.
- Selective Estrogen Receptor Modulators (SERMs): These newer therapies, such as tamoxifen and raloxifene, offer targeted effects on estrogen receptors in different tissues, providing potential benefits in hormone-dependent gynecological cancers and bone health.
- Progestins: Synthetic progestins can be used to prevent preterm delivery in high-risk women, manage abnormal uterine bleeding, and treat endometrial hyperplasia and carcinoma
Drugs for Pregnancy, Labor, and Delivery
A specific class of drugs is used to control uterine activity during pregnancy and labor
- Uterine Stimulants (Oxytocics): These drugs increase uterine motility and are used to induce labor, augment slow labor, induce abortion, and prevent/treat postpartum hemorrhage.
- Oxytocin: A nona-peptide hormone, it works by activating oxytocin receptors (OTR) in the myometrium, which increases intracellular calcium levels and enhances contractions. It is the uterotonic drug of choice recommended by the WHO for preventing postpartum hemorrhage.
- Prostaglandins: Agents like dinoprostone (Prostin E2) and misoprostol increase intramyometrial calcium concentrations to promote contractions and are used for cervical ripening and medical termination of pregnancy.
- Ergot Alkaloids: Drugs such as methylergonovine maleate (Methergine) cause strong, continuous uterine contractions and are primarily used to prevent and treat postpartum and post-abortion hemorrhage.
- Uterine Relaxants (Tocolytics): These agents decrease uterine motility to suppress preterm labor.
- Magnesium Sulfate: Though its exact mechanism in tocolysis is not fully defined, it is a CNS depressant also used as an anticonvulsant to manage seizures in severe pre-eclampsia and eclampsia.
- Calcium Channel Blockers: Nifedipine is an example of a calcium channel blocker used to relax the myometrium and delay preterm delivery.
- Oxytocin Receptor Antagonists: Atosiban, a competitive inhibitor of OTR, binds to the receptors to prevent oxytocin’s effects, thus inhibiting contractions
Anti-infective Agents
Various antimicrobial agents are used to treat genital and pelvic infections.
- Antifungals: Drugs like clotrimazole, miconazole, and butoconazole are used topically to treat vulvovaginal candidiasis.
- Antibiotics: Metronidazole is an agent used to treat trichomoniasis and bacterial vaginosis, as well as anaerobic bacterial infections. Systemic antibiotics are often used for pelvic inflammatory disease
Pregnancy & Lactation Care for Gynecology Course
Care during pregnancy and lactation requires balancing the therapeutic needs of the mother with potential risks to the developing fetus or nursing infant. Modern guidelines prioritize individualized risk-benefit analyses over older, simplified grading systems.
Pregnancy Care & Pharmacology
Prescribing during pregnancy is complex due to physiological changes that alter drug Pharmacokinetics (PK).
Physiological Changes:
Absorption: Delayed gastric emptying and vomiting can alter oral drug uptake.
Distribution: Plasma volume increases by 40%, potentially diluting drug concentrations, while reduced albumin levels can increase the “free” or active portion of highly protein-bound drugs.
Metabolism & Elimination: Renal blood flow and glomerular filtration rate (GFR) increase by up to 50–80%, leading to faster clearance of drugs like cephalosporins.
Safety Labeling (PLLR): The FDA replaced the A, B, C, D, X letter categories with the Pregnancy and Lactation Labeling Rule (PLLR), which uses narrative summaries of human and animal data to guide clinical decisions.
Essential Medications:
- Supplements: Iron and folic acid are routinely recommended to prevent anemia.
- Pre-eclampsia Prevention: Low-dose aspirin and calcium may be prescribed for high-risk women.
- Emergency Care: Magnesium sulfate remains the standard for managing seizures in eclampsia
Lactation Care & Pharmacology
Most medications are compatible with breastfeeding because the dose transferred into milk is typically much lower than what is considered safe for direct infant use. National Institutes of Health (NIH) | (.gov)
- Drug Transfer Principles: Factors like high lipid solubility, low molecular weight, and low protein binding increase a drug’s likelihood of entering breast milk.
- Safe Common Medications:
- Pain Relief: Paracetamol (Tylenol) and ibuprofen are considered first-line and safe.
- Antibiotics: Penicillins (amoxicillin) and cephalosporins are generally safe.
- Contraception: Progestin-only “mini-pills” are preferred over combined estrogen-progestin pills, which may reduce milk supply.
- Contraindicated or Cautioned Drugs:
- Avoid: Anti-cancer drugs (antineoplastics), lithium, oral retinoids, and amiodarone.
- Caution: Pseudoephedrine (found in cold medicines) may reduce milk supply. Codeine should be avoided due to the risk of excessive sedation or respiratory depression in the infant.
Gynecological Disease & Treatment for Gynecology Course
Gynecological diseases affect the female reproductive system (uterus, ovaries, fallopian tubes, vagina, vulva), caused by infections, hormonal imbalances, genetics, or cancer, leading to symptoms like pain, irregular bleeding, and infertility. Treatments include medication (antibiotics, hormones), lifestyle changes, and surgical interventions such as laparoscopy or hysterectomy. Regular check-ups, including Pap smears and HPV vaccines, are crucial for prevention and early diagnosis.
Common Gynecological Diseases & Conditions
- Infections: Vaginal candidiasis (yeast infections), bacterial vaginosis, and sexually transmitted infections (STIs).
- Structural Issues: Uterine fibroids (myomas), ovarian cysts, endometrial polyps, and uterine prolapse.
- Hormonal & Functional Disorders: Polycystic Ovary Syndrome (PCOS), endometriosis, and adenomyosis.
- Menstrual Disorders: Amenorrhea (absent periods), heavy bleeding (menorrhagia), or painful periods (dysmenorrhea).
- Cancers: Cervical, ovarian, and endometrial cancer.
- Others: Urinary incontinence, vaginal atrophy (menopause), and Vaginismus.
Diagnostic Procedures
- Pelvic Exam & Pap Smear: For checking for infections, abnormalities, and cervical cancer.
- Ultrasound: Transvaginal or pelvic ultrasound to detect cysts, fibroids, and structural issues.
- Blood Tests: To analyze hormone levels (e.g., for PCOS, thyroid).
- Hysteroscopy/Laparoscopy: Minimally invasive, direct visualization of the uterus or pelvic cavity.
Treatment Approaches
- Medication Therapy: Antibiotics for infections, hormonal birth control for regulating periods/endometriosis, and painkillers.
- Surgery: Minimally invasive techniques (hysteroscopy, laparoscopy) to remove cysts, polyps, or fibroids, or more extensive surgeries like hysterectomy.
- Lifestyle Modifications: Diet and exercise to manage conditions like PCOS and obesity-related issues.
- Specialized Treatments: Laser therapy or PRP for vaginal atrophy, and fertility treatments (IVF
Gynecological Surgery for Gynecology Course
স্ত্রীরোগ সংক্রান্ত অস্ত্রোপচারে মহিলাদের প্রজনন ব্যবস্থা – জরায়ু, ডিম্বাশয়, ফ্যালোপিয়ান টিউব, জরায়ু এবং শ্রোণী – – এর উপর অস্ত্রোপচার পদ্ধতি জড়িত থাকে যাতে সৌম্য অবস্থা (ফাইব্রয়েড, এন্ডোমেট্রিওসিস), ক্যান্সার, বন্ধ্যাত্ব বা অসংযম চিকিৎসা করা যায়। আধুনিক কৌশলগুলি দ্রুত আরোগ্য, কম ব্যথা এবং ঐতিহ্যবাহী ওপেন সার্জারির (ল্যাপারোটমি)তুলনায় ছোট ছেদনের জন্য ন্যূনতম আক্রমণাত্মক পদ্ধতি (ল্যাপারোস্কোপি, রোবোটিক্স) এর উপর জোর দেয়.
সাধারণ স্ত্রীরোগ সংক্রান্ত পদ্ধতি
- হিস্টেরেক্টমি: জরায়ু অপসারণ (মোট বা সাবটোটাল), কখনও কখনও ডিম্বাশয় (ওফোরেক্টমি) বা ফ্যালোপিয়ান টিউব সহ।
- ল্যাপারোস্কোপি/রোবোটিক সার্জারি: কীহোল, বিভিন্ন অস্ত্রোপচারের জন্য ন্যূনতম আক্রমণাত্মক পদ্ধতি।
- মায়োমেকটমি: জরায়ু সংরক্ষণের সময় জরায়ু ফাইব্রয়েড অপসারণ।
- ডিম্বাশয়ের সিস্টেক্টমি/ ওফোরেক্টমি: ডিম্বাশয়ের সিস্ট বা ডিম্বাশয় নিজেই অপসারণ।
- হিস্টেরোস্কোপি: জরায়ুর আস্তরণ পরীক্ষা/চিকিৎসার জন্য জরায়ুর মধ্য দিয়ে ক্যামেরা ব্যবহার করা।
- টিউবাল লাইগেশন: স্থায়ী গর্ভনিরোধক।
- পেলভিক ফ্লোর মেরামত: প্রোল্যাপস বা অসংযমের চিকিৎসা।
Abortion for Gynecology Course
Abortion is the medical, intentional termination of a pregnancy before the fetus can survive outside the uterus. It is a common, safe procedure, often considered 14 times safer than childbirth. Abortions are divided into two main categories—medication and procedural (or surgical)—depending on gestational age.
. 1. Types of Abortion Methods
- Medication Abortion (The “Abortion Pill”): Typically used in the first trimester (up to 70-77 days of gestation). It involves taking two different medicines, mifepristone and misoprostol, which cause the uterus to shed its lining and expel the pregnancy, similar to a miscarriage.
- Procedural Abortion (In-Clinic): Performed by a doctor in a clinic or hospital.
- Vacuum Aspiration: Used up to 14–16 weeks gestation, this method uses gentle suction to empty the uterus.
- Dilation and Evacuation (D&E): Used for more advanced pregnancies, typically after 14–16 weeks
2. Safety and Risks
- Safety: When performed by trained professionals, abortions are highly safe with very low complication rates.
- Risks: Complications are rare but can include heavy bleeding, infection, or incomplete removal of tissue (requiring a follow-up procedure).
- Fertility: Having a safe, legal abortion does not affect future fertility
3. Procedures and What to Expect
- Before: Providers often perform a medical history, ultrasound, or blood tests to determine gestational age and ensure it is not an ectopic pregnancy.
- During: A medication abortion involves cramping and bleeding at home. A procedural abortion takes 5–10 minutes, usually with local anesthesia, and patients often go home the same day.
- After: Cramping and bleeding, similar to a period, can last for a week or two
4. Legal Status and Access
- Global Access: As of 2018, about 37% of the world’s women had access to legal abortions without limits on reason, though laws differ by country.
- Unsafe Abortion: Unsafe abortions occur where legal access is restricted, resulting in significantly higher maternal morbidity and mortality.
- United States: Since the 2022 Supreme Court ruling Dobbs v. Jackson, there is no national right to abortion; laws vary significantly by state, ranging from total bans to full access
Missccarriage for Gynecology Course
A miscarriage is the spontaneous loss of a pregnancy before 24 weeks, most commonly occurring within the first trimester (under 12 weeks). Common symptoms include vaginal bleeding, abdominal pain, and cramping, sometimes with no symptoms appearing at all until a routine scan. While often caused by random chromosomal issues, other factors include age, infections, and health conditions. Treatment options include allowing the tissue to pass naturally (“watchful waiting”), medication, or surgical procedures.
Miscarriage symptoms, common in the first trimester, typically include vaginal bleeding (ranging from spotting to heavy flow), abdominal or pelvic cramping, and lower back pain. Other signs include passing tissue, a sudden reduction in pregnancy symptoms like nausea or breast tenderness, and dizziness. If you experience these symptoms, contact a healthcare provider immediately.
Common Early Signs and Symptoms
- Vaginal Bleeding: Often the first sign, ranging from light spotting to heavy bleeding with clots.
- Abdominal/Pelvic Pain: Cramping that may feel like intense menstrual cramps, often on one side.
- Lower Back Pain: A dull ache or pressure in the lower back.
- Passing Tissue: Passing gray or blood-like tissue or fluid from the vagina.
- Disappearance of Symptoms: A sudden loss of pregnancy signs, such as decreased breast tenderness, reduced nausea, or feeling less pregnant.
When to Seek Medical Attention
- Heavy Bleeding: Soaking through pads quickly.
- Severe Pain: Intense, persistent abdominal pain or dizziness/fainting.
- Fever/Chills: These can indicate an infection
Miscarriage types, which represent pregnancy loss before 20-24 weeks, are classified by symptoms and the status of the pregnancy tissue. Key types include threatened (bleeding, closed cervix), inevitable (open cervix), complete (all tissue passed), incomplete (some tissue remains), and missed (fetal death without immediate symptoms). Other types include chemical pregnancies, recurrent losses, and rare septic infections.
Key Types of Miscarriage Explained:
- Threatened Miscarriage: Characterized by vaginal bleeding and sometimes cramps, but the cervix remains closed. The pregnancy may continue normally, or it may progress to an inevitable miscarriage.
- Inevitable Miscarriage: The symptoms (bleeding, cramping) are stronger, and the cervix is open, indicating the miscarriage cannot be prevented.
- Incomplete Miscarriage: Some pregnancy tissue has passed from the uterus, but some remains. This often requires medical intervention to remove the remaining tissue.
- Complete Miscarriage: All products of conception (tissue) have left the uterus. This is often confirmed via ultrasound and usually occurs in the first trimester.
- Missed Miscarriage: The fetus has passed away or did not develop, but the body has not recognized the loss or expelled the tissue, often having no symptoms.
- Chemical Pregnancy: An early loss occurring within the first 5 weeks, often before a heartbeat is detected.
- Recurrent Miscarriage: Defined as experiencing three or more consecutive first-trimester miscarriages.
- Septic Miscarriage: A rare, serious infection of the uterine tissue that occurs during a miscarriage, requiring immediate medical care.
- Blighted Ovum (Anembryonic Pregnancy): A fertilized egg attaches to the uterus, but the embryo does not develop
Common Symptoms:
- Vaginal bleeding or spotting (can be light or heavy).
- Abdominal cramps or pain in the lower back.
- Passing of tissue
Family Planning
Family planning is a comprehensive medical and social field that enables individuals and couples to determine the number and spacing of their children. It extends beyond pregnancy prevention to include infertility treatments, reproductive health counseling, and the prevention of sexually transmitted infections (STIs).
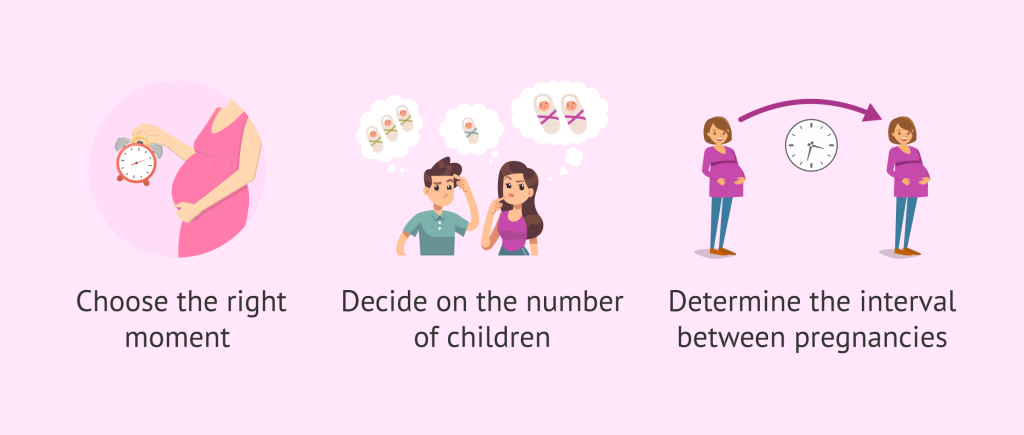
Core Educational Objectives
The subject of family planning focuses on several critical pillars of reproductive health and societal well-being:
- Birth Spacing: Recommending intervals of at least 24 to 36 months between births to allow the mother’s body to recover and ensure better health outcomes for the infant.
- Maternal & Child Health: Reducing high-risk pregnancies (e.g., those occurring in mothers “too young” or “too old”) to lower maternal and infant mortality rates.
- Infertility Management: Providing counseling and medical interventions, such as Assisted Reproductive Technology (ART), for those struggling to conceive.
- Empowerment: Ensuring individuals have the autonomy to complete education and pursue economic opportunities by managing their reproductive life cycle
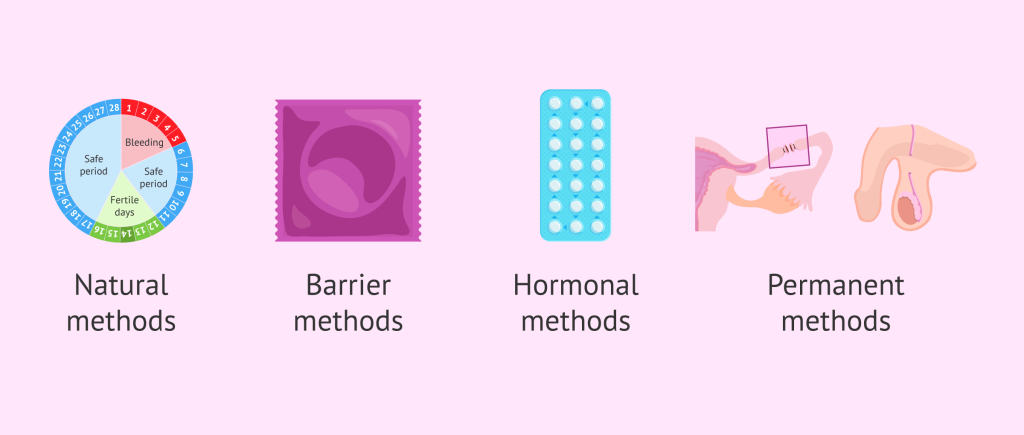
Categories of Contraceptive Methods
A primary focus of the subject is the mechanism and efficacy of various contraceptive methods:
| Category | Methods | Mechanism | Efficacy (Typical) |
|---|---|---|---|
| Long-Acting Reversible (LARC) | IUDs, Implants | Hormonal or physical barrier to fertilization | ~99% |
| Hormonal (Short-Acting) | Pills, Injections, Patches | Suppress ovulation and thicken cervical mucus | 93–96% |
| Barrier | Condoms, Diaphragms | Physically block sperm; condoms also prevent STIs | 79–87% |
| Permanent | Vasectomy, Tubal Ligation | Surgical blocking of sperm or egg pathways | >99% |
| Natural/Behavioral | Fertility Awareness, LAM | Tracking ovulation or using breastfeeding cues | Variable; LAM ~98% |
Counseling and Service Delivery
Comprehensive family planning services are delivered through multiple modes to ensure accessibility
- Facility-Based: Specialized care in hospitals and clinics for medically complex procedures like IUD insertion or sterilization.
- Community-Based: Distribution of oral pills and condoms by trained community health workers or extension practitioners.
- Youth-Friendly Services: Tailoring care for adolescents to provide confidential, non-judgmental counseling and education.
- Integrated Care: Combining family planning with other services such as HIV/STI screening, post-abortion care, and prenatal visits.
Global & Individual Impact
- Economic: Every $1 invested in family planning can yield nearly $27 in long-term economic benefits by reducing healthcare costs and boosting workforce participation.
- Environmental: By helping manage population growth, family planning is considered a significant action against climate change and resource depletion.
- Human Rights: Access to voluntary family planning is recognized globally as a fundamental human right essential for gender equality
Menstrual Cycle & Disorders for Gynecology Course
The menstrual cycle is a rhythmic series of biological events—typically lasting between 21 and 35 days—that prepares the body for potential pregnancy. This cycle is orchestrated by a delicate balance of hormones secreted by the brain (pituitary gland) and the ovaries.
Phases of the Menstrual Cycle
The cycle is commonly divided into four phases based on ovarian and uterine activity:
| Phase | Timing (Approx.) | Key Hormonal Shifts | Physical/Biological Events |
|---|---|---|---|
| Menstrual | Days 1–5 | Estrogen & Progesterone drop | Shedding of the uterine lining (the period); typically lasts 3–7 days. |
| Follicular | Days 1–14 | FSH rises | The pituitary gland releases FSH to stimulate egg-containing follicles in the ovaries. |
| Ovulation | Day 14 | LH surge | A sharp spike in LH triggers the dominant follicle to release a mature egg. |
| Luteal | Days 15–28 | Progesterone peaks | The empty follicle becomes the corpus luteum, producing progesterone to thicken the uterine lining. |
Common Menstrual Disorders
Menstrual disorders refer to abnormalities in the cycle’s frequency, flow, or associated symptoms. Dysmenorrhea: Frequent and intense menstrual cramps. Primary dysmenorrhea occurs without an underlying condition, while secondary is often due to medical issues like endometriosis or fibroids.
Amenorrhea: The absence of a period. It is primary if menstruation hasn’t started by age 15–16 and secondary if periods stop for 3+ months.
Menorrhagia (Heavy Bleeding): Bleeding that lasts longer than 7 days or requires changing sanitary products every 1–2 hours.
Oligomenorrhea & Polymenorrhea: Irregular cycle lengths; oligomenorrhea refers to cycles longer than 35 days, while polymenorrhea refers to cycles shorter than 21 days.
PMS & PMDD: Physical and emotional changes before menstruation. Premenstrual Dysphoric Disorder (PMDD) is a more severe form characterized by intense anxiety, depression, or irritability.
When to Consult a Professional
Occasional irregularity is common during puberty, stress, or perimenopause, but persistent issues should be evaluated. Seek medical advice if you experience.
- Periods that abruptly stop for more than 3 months.
- Severe pain that interferes with daily activities.
- Bleeding between periods or after sexual intercourse.
- Signs of anemia, such as extreme fatigue or dizziness, due to heavy flow.
Pediatric and Adolescent Gynecology (PAG)
Pediatric and Adolescent Gynecology (PAG) is a specialized medical field focusing on the reproductive health of girls from birth through adolescence. It addresses unique anatomical, hormonal, and developmental conditions—such as menstrual disorders, infections, and congenital abnormalities—requiring tailored,, sensitive care that often involves family collaboration, and specialized surgical skills
ey Aspects of PAG:
- Specialized Training: Practitioners are usually OB/GYNs with additional, focused training (1–2 years) in pediatric and adolescent needs.
- Scope of Care: Covers a wide range of issues from birth to young adulthood, including vulvar skin concerns in toddlers, puberty disorders, adolescent endometriosis, menstrual issues, and contraception.
- Multidisciplinary Approach: Often involves collaboration with pediatric endocrinologists, surgeons, and geneticists.
- Patient-Centered Approach: Focuses on creating a comfortable environment, building trust, and ensuring confidentiality for teenagers
Common Conditions Treated:
- Pre-pubertal: Labial adhesions, genital injuries, infections, and congenital malformations.
- Adolescent: Menstrual dysfunction (heavy/irregular), amenorrhea, PCOS, endometriosis, ovarian cysts, and breast issues
 HRTD Medical Institute HRTD Medical Institute
HRTD Medical Institute HRTD Medical Institute



