Diploma In Pharmacy Course 1 Year Details
Diploma In Pharmacy Course 1 Year. Mobile Phone 01797522136, 01987073965. The 1 Year Pharmacy Course is short in Bangladesh. This Pharmacy Course 1 Year is helpful for passing the C Grade Pharmacy Technician Course Exam ( C Grade Pharmacist Exam). This course is also helpful for running a Medicine Business or Pharmacy Business. This one-year pharmacy course helps obtain a Visa to go abroad. There are 10 subjects and Many Practical Works in this course. The Pharmacy Course 1 Year is available in HRTD Medical Institute. HRTD Medical Institute is an organization of HRTD Limited, which is registered by the Government of the People’s Republic of Bangladesh. This HRTD Medical Institute is a Training Institute in the Medical Sector.

ফার্মেসি কোর্স ১ বছরের বাংলাদেশে একটি সংক্ষিপ্ত ফার্মেসি কোর্স। এই ফার্মেসি কোর্স ১ বছরের সি গ্রেড ফার্মেসি টেকনিশিয়ান কোর্স পরীক্ষা (সি গ্রেড ফার্মাসিস্ট পরীক্ষা) পাস করার জন্য সহায়ক। এই কোর্সটি মেডিসিন ব্যবসা বা ফার্মেসি ব্যবসা পরিচালনার জন্যও সহায়ক। এই ফার্মেসি কোর্স ১ বছরের বিদেশ ভ্রমণের জন্য ভিসা নেওয়ার জন্য সহায়ক। এই কোর্সে ১০টি বিষয় এবং অনেক ব্যবহারিক কাজ রয়েছে।
Location for Diploma In Pharmacy Course 1 Year in Dhaka, Bangladesh
Location of Diploma In Pharmacy Course 1 Year.Mobile Number.01987073965.01797522136,HotLine-01969947171 HRTD Medical Institute , Abdul Ali Madbor Mention, Section-6, Block-Kha, Road-1, Plot-11, Mirpur-10 (Gol-Chattar) Metro Rail Pilar NO-249, Dhaka-1216. It is situated by the West Side of Agrani Bank, the South Side of Fire Service, Islami Bank, Janata Bank, Social Islami Bank, Medinova, Ibrahim Diabetic Hospital, the North Side of Baitul Mamur Jame Mosjid, Grave of Baitul Mamur Jame Mosjid, and East Side of Maliha Apartment.
এইচআরটিডি মেডিকেল ইনস্টিটিউট, আব্দুল আলী মাদবর ম্যানশন, সেকশন-6, ব্লক-খা, রোড-1, প্লট-11, মেট্রো রেল পিলার নং 249, ফলপট্টি মসজিদ গলি, মিরপুর-10 গোলচত্তর, ঢাকা-1216।
Hostel Facilities in HRTD Medical Institute
Hostel & Meal Facilities
The Institute has hostel facilities for the students. Students can take a bed in the hostel.
Hostel Fee Tk 3000/- Per Month
Meal Charges Tk 3000/- Per Month. ( Approximately )
হোস্টাল ও খাবার সুবিধা
ইনস্টিটিউটে শিক্ষার্থীদের জন্য হোস্টেল সুবিধা রয়েছে। ছাত্ররা হোস্টেলে বিছানা নিতে পারে।
হোস্টেল ফি 3000/- টাকা প্রতি মাসে,
খাবারের চার্জ 3000/- টাকা প্রতি মাসে।(প্রায়)
Teachers For Diploma In Pharmacy Course 1 Year
- Dr. Md. Sakulur Rahman, MBBS, CCD (BIRDEM), Course Director
- Dr. Sanjana Binte Ahmed, BDS, MPH, Assistant Course Director
- Dr. Tisha, MBBS, PGT Gyne, Assistant Course Director
- Dr. Suhana, MBBS, PGT Medicine
- Dr. Danial Hoque, MBBS, C-Card
- Dr. Tisha, MBBS
- Dr. Afrin Jahan, MBBS, PGT Medicine
- Dr. Ananna, MBBS
- Dr. Lamia Afroze, MBBS
- Dr. Amena Afroze Anu, MBBS, PGT Gyne, Assistant Course Director
- Dr. Farhana Antara, MBBS,
- Dr. Nazmun Nahar Juthi, BDS, PGT
- Dr. Farhana Sharna, MBBS
- Dr. Bushra, MBBS
- Dr. Turzo, MBBS
- Dr. Kamrunnahar Keya, BDS, PGT (Dhaka Dental College)
- Dr. Shamima, MBBS, PGT Gyne
- Dr. Alamin, MBBS
- Dr. Benzir Belal, MBBS
- Dr. Disha, MBBS
- Dr. Mahinul Islam, MBBS
- Dr. Tisha, MBBS, PGT Medicine
- Dr. Anika, MBBS, PGT
- Dr. Jannatul Ferdous, MBBS, PGT Gyne
- Dr. Jannatul Aman, MBBS, PGT
- Dr. Rayhan, BPT
- Dr. Abu Hurayra, BPT
- Dr. Sharmin Ankhi, MBBS, PGT Medicine
- Md. Monir Hossain, B Pharm, M Pharm
- Md. Monirul Islam, B Pharm, M Pharm
- Md. Feroj Ahmed, BSc Pathology, PDT Medicine
Practical Class For Diploma In Pharmacy Course 1 Year
- Heart Beat, Heart Rate
- Heart Sound,Pulse
- Blood Pressure, Hypertension, Hypotension
- First Aid Box
- Auscultation
- Inhaler, Rotahaler
- Nebulizer
- Glucometer Blood Glucose
- Injection I/V
- Injection I/M
- Cleaning,Dressing,Bandaging
- Saline
- CPR
- Stitch
- Body Temperature
- Nasal Tube Gel ,Hand Wash
- Blood Grouping
- Cyanosis, Dehydration Test, Edema Test
Subjects for Diploma In Pharmacy Course 1 Year
Diploma In Pharmacy Course 1 Year .This Course Contains 10 Subjects.
- Human Anatomy and Physiology
- General Chemistry and Pharmacology-1
- First Aid and Study of OTC Drugs
- Pharmacology-2
- Medical Diagnosis
- Practice of Medicine
- Respiratory and Digestive Drugs
- Cardiovascular Drugs
- Hormonal and Antidiabetic Drugs
- Pediatric Drugs
Some Practical Class Details Given Below for Diploma In Pharmacy Course 1 Year
Blood Pressure Practical
Blood pressure is recorded as two numbers, such as 120/80. The larger number is the pressure in the arteries as the heart pumps out blood during each beat. This is called the systolic blood pressure. The lower number is the pressure as the heart relaxes before the next beat.
Systolic BP / Diastolic BP
Example: 120/80 mmHg
Types of Blood Pressure
1. Systolic Blood Pressure (SBP)
- Pressure during ventricular contraction (systole)
- Normal: 120 mmHg
2. Diastolic Blood Pressure (DBP)
- Pressure during ventricular relaxation (diastole)
- Normal: 80 mmHg
Normal Blood Pressure Values (Adults)
| Category | Systolic (mmHg) | Diastolic (mmHg) |
|---|---|---|
| Normal | 90–120 | 60–80 |
| Pre-Hypertension | 121–139 | 81–89 |
| Hypertension Stage 1 | 140–159 | 90–99 |
| Hypertension Stage 2 | ≥160 | ≥100 |
| Hypotension | <90 | <60 |
Abnormal Blood Pressure
1. Hypertension
Persistently elevated BP
Causes:
- Primary (essential)
- Secondary (renal, endocrine)
Complications:
- Stroke
- Heart attack
- Kidney failure
- Retinopathy
2. Hypotension
Low blood pressure
Causes:
- Dehydration
- Blood loss
- Shock
- Heart failure
Symptoms:
- Dizziness
- Fainting
- Weak pulse
Heart Beat
Definition
A heart beat is one complete cycle of contraction (systole) and relaxation (diastole) of the heart.
- Each beat pumps blood to the body
- Controlled by the cardiac conduction system
Heart Rate (HR)
Definition
Heart Rate is the number of heart beats per minute (bpm).
Example:
- 72 beats/minute = normal adult resting heart rate
Normal Heart Rate Values
Adults
- 60–100 bpm
Children
- 70–120 bpm
Infants
- 120–160 bpm
Athletes
- 40–60 bpm (normal due to strong heart)
Types of Heart Rate
1. Tachycardia
- HR > 100 bpm
- Causes: fever, exercise, stress, anemia
2. Bradycardia
- HR < 60 bpm
- Causes: athletes, hypothermia, heart block
Nebulizer Practical for Diploma In Pharmacy Course 1 Year
Definition
A nebulizer is a medical device that converts liquid medicine into a fine mist (aerosol) so that it can be inhaled directly into the lungs.
Purpose of Nebulizer
- To deliver medicine directly to the respiratory tract
- Useful when patients cannot use inhalers properly
- Provides quick relief in breathing problems
Common Uses
- Asthma
- COPD (Chronic Obstructive Pulmonary Disease)
- Bronchitis
- Pneumonia
- Acute respiratory distress
- Wheezing in children
- Emergency shortness of breath
Types of Nebulizer
1. Jet Nebulizer
- Uses compressed air
- Most commonly used
- Affordable
2. Ultrasonic Nebulizer
- Uses ultrasonic vibrations
- Quiet operation
- Faster drug delivery
3. Mesh Nebulizer
- Uses vibrating mesh
- Portable
- Efficient and expensive
Parts of a Nebulizer
- Air compressor
- Nebulizer cup (medicine chamber)
- Mouthpiece or face mask
- Tubing
Common Drugs Used in Nebulization
- Salbutamol (Albuterol) – bronchodilator
- Ipratropium bromide
- Budesonide
- Normal saline
- Antibiotics (in some cases)
Procedure of Nebulization
- Wash hands
- Measure prescribed medicine
- Pour medicine into nebulizer cup
- Connect tubing to compressor
- Place mask/mouthpiece properly
- Switch on the machine
- Patient breathes slowly and deeply
- Continue until mist stops (5–10 minutes)
- Clean equipment after use
Advantages
- Easy to use
- Suitable for children and elderly
- Direct action on lungs
- Less systemic side effects
Disadvantages
- Bulky (except portable types)
- Requires electricity
- Longer time than inhalers
Side Effects
- Tremors
- Palpitations
- Dry mouth
- Throat irritation
- Rare allergic reactions
Glucometer Blood Glucose Practical For Diploma In Pharmacy Course 1 Year
A glucometer (blood sugar meter) is a portable medical device that measures the amount of sugar (glucose) in a drop of blood, essential for managing diabetes by helping you see how food, exercise, and medicine affect your levels, typically using a finger prick and a test strip to get a reading in mg/dL or mmol/L within seconds. To use, you prick your finger (after washing hands), touch the blood to a test strip, and the meter displays your blood sugar level, guiding treatment and preventing complications.
How it Works
- Prepare: Wash hands, insert a test strip into the meter (this turns it on).
- Lancet: Prepare a lancet device, setting the depth and loading it.
- Prick: Firmly press the lancet on the side of your fingertip and squeeze a small blood drop.
- Apply Blood: Touch the drop to the edge of the test strip.
- Read: The meter counts down and displays the glucose level (e.g., 80-130 mg/dL is a common target before meals).
Key Things to Know
- Purpose: To manage diabetes by tracking glucose levels, preventing highs (hyperglycemia) and lows (hypoglycemia).
- Components: A handheld meter, disposable test strips, and lancets.
- Accuracy: Store strips properly (sealed, room temp) and check expiration dates; a small drop of blood is needed.
- When to Use: People with diabetes use them multiple times daily to guide treatment.
Target Ranges (General Guidelines)
- Before Meals (Preprandial): 80-130 mg/dL.
- After Meals (Postprandial): Less than 180 mg/dL (2 hours after starting to eat).
Pulse in the Human Body Practical Class for Diploma In Pharmacy Course 1 Year
A pulse in the human body is the rhythmic expansion and contraction of arteries as blood is pumped through by the heart, essentially your heart rate (beats per minute) felt at various points (like the wrist or neck). A normal resting pulse for adults is 60-100 beats per minute, but it varies with age, fitness, emotions, and activity, reflecting overall cardiovascular health, with fast (tachycardia) or slow (bradycardia) rates potentially signaling issues.
What it is
- A wave of pressure: Each heartbeat sends blood through the arteries, causing them to expand and contract, creating the pulse you feel.
- A vital sign: Measuring it tells you your heart rate (how many times it beats per minute) and can reveal rhythm and strength.
Common pulse points
- Radial artery: Inside of the wrist, at the base of the thumb.
- Carotid artery: Side of the neck.
- Brachial artery: Inside of the upper arm, near the elbow.
- Femoral artery: In the groin.
- Popliteal artery: Behind the knee.
- Temporal artery: Near the temples, just above the ear.
What affects your pulse rate
- Normal factors: Age, fitness level (athletes can have very low resting rates), stress, emotions, body position, fever, caffeine, and nicotine.
- Health indicators: A consistently high rate (tachycardia) or low rate (bradycardia) could signal underlying problems like thyroid issues, anemia, or heart conditions, requiring medical evaluation.
Pulse Rate Practical Class for Diploma In Pharmacy Course 1 Year
Your pulse rate (or heart rate) is how many times your heart beats per minute, with a normal resting rate for adults typically 60-100 beats per minute (bpm), but it varies by age, fitness, stress, and medications, with athletes often having lower rates and babies/children having higher rates. You can check it by feeling your pulse on your wrist or neck and counting beats for 15 seconds, then multiplying by four, or use a fitness tracker for instant readings.
Normal Resting Heart Rates by Age (approximate)
- Newborns (Birth-4 weeks): 100–205 bpm
- Infants (4 weeks-1 year): 100–180 bpm
- Toddlers (1-3 years): 98–140 bpm
- School Age (5-12 years): 75–118 bpm
- Adolescents (13-17 years): 60–100 bpm
- Adults (18+ years): 60–100 bpm (athletes can be 40-60 bpm)
What Affects Your Pulse Rate?
- Physical Activity: Increases with exertion.
- Stress/Emotions: Anxiety or excitement raises it.
- Body Position: Lower when lying down, higher when standing.
- Medications: Beta-blockers can lower it.
- Health Conditions: Fever, infection, or heart problems can affect it.
Weak Pulse Practical Class for Diploma In Pharmacy Course 1 Year
A weak pulse means your arteries aren’t expanding strongly with each heartbeat, often felt as thready or difficult to find, and can signal serious issues like shock or heart problems, requiring immediate emergency care if accompanied by dizziness, fainting, chest pain, or confusion, though it can sometimes just be normal for very fit people. It’s usually caused by the heart not pumping enough blood (low stroke volume) due to electrical issues (bradycardia, sick sinus), severe dehydration, blood loss, or peripheral artery disease (PAD) in the limbs, which needs urgent medical assessment.
Common Causes of a Weak Pulse
- Low Heart Rate (Bradycardia): Heart beats less than 60 bpm, common in athletes but can signal heart disease.
- Heart Rhythm Problems (Arrhythmias): Electrical signals are disrupted, leading to slow or irregular beats.
- Shock: Severe drop in blood flow, from dehydration, blood loss, or heart failure.
- Peripheral Artery Disease (PAD): Narrowed arteries in the legs/feet reduce blood flow.
- Dehydration/Blood Loss: Not enough fluid volume for strong beats.
- Medications: Some drugs (like beta-blockers) can slow the heart rate.
- Thyroid Issues: An underactive thyroid (hypothyroidism) can slow metabolism and heart rate.
When to Seek Emergency Care (Call 911/Emergency Services)
If you or someone else has a weak pulse along with any of these severe symptoms, get help immediately:
- Fainting or near-fainting
- Severe dizziness or confusion
- Shortness of breath
- Chest pain
- Difficulty speaking or moving
What to Do
- Assess Severity: Is it just slow (athlete) or weak/thready (emergency)?
- Check Other Symptoms: Look for signs of shock or heart distress.
- Seek Medical Help: A weak pulse is often serious; consult a doctor or go to the ER.
Cleaning Process in First Aid for Diploma In Pharmacy Course 1 Year
The first aid wound cleaning process involves washing your hands, rinsing the wound gently under cool running water to remove dirt, cleaning around the wound with mild soap (avoiding inside), patting dry with clean gauze/cloth, and then applying ointment and a sterile bandage, all to prevent infection and promote healing, while avoiding harsh antiseptics like hydrogen peroxide.
Step-by-Step Cleaning Process
- Wash Your Hands: Before touching the wound, thoroughly wash and dry your hands to prevent introducing bacteria.
- Stop Bleeding (if needed): Apply gentle, direct pressure with a clean cloth or sterile gauze until bleeding slows.
- Rinse the Wound: Place the wound under cool, running tap water to flush out dirt and debris.
- Clean Around the Wound: Use mild soap and a clean cloth/gauze to wash the skin around the wound, wiping away from the center.
- Remove Debris: Gently remove any visible dirt with clean, alcohol-swabbed tweezers; don’t dig or scrub.
- Pat Dry: Gently pat the area dry with a clean cloth or sterile gauze; avoid rubbing.
- Apply Ointment: Apply a thin layer of antibiotic ointment or petroleum jelly to keep the surface moist (optional, but helps prevent scarring).
- Cover the Wound: Apply a sterile bandage or gauze to keep it clean and protected, changing it daily or if it gets wet/dirty.
What to Avoid
- Rubbing: Can irritate the skin and damage tissue.
- Harsh Antiseptics: Avoid hydrogen peroxide, iodine, or alcohol directly in the wound as they can damage skin and slow healing.
- Ice: Don’t use ice on burns; use cool water instead.
When to Seek Medical Help
- Bleeding won’t stop.
- Deep puncture or embedded objects.
- Human or animal bites.
- Signs of infection (increased redness, swelling, pus).
- Uncertainty about tetanus vaccination.
Dressing Process in First Aid for Diploma In Pharmacy Course 1 Year
The first aid dressing process involves hygiene, stopping bleeding, cleaning the wound, applying a sterile pad, and securing it with a bandage, all while preventing infection by washing hands and wearing gloves. Key steps include washing hands, wearing gloves, placing a pad larger than the wound, securing it with tape/bandage, and checking circulation, ensuring it’s snug but not too tight.
Steps for Applying a Dressing
- Prepare:
- Stay calm and ensure the scene is safe.
- Wash your hands thoroughly and put on disposable gloves to prevent infection.
- If bleeding, apply direct pressure with a clean cloth until it slows.
- Clean the Wound (if possible):
- Rinse the wound with clean, cold water to remove dirt.
- Gently pat the surrounding skin dry.
- Do not remove embedded objects; leave them for medical staff.
- Apply the Dressing:
- Choose a dressing pad slightly larger than the wound.
- Hold the bandage part (not the pad) and place the sterile pad directly over the wound, ensuring it covers the entire area.
- If using a dressing with an attached bandage, wrap the short end around the limb, then the long end in the opposite direction.
- Secure the pad by tying the bandage ends over the pad in a reef knot (square knot).
- For roller bandages, start below the wound, overlap turns by two-thirds, and secure at the end with tape or a pin.
- Check Circulation:
- Press a fingernail or skin beyond the dressing; it should turn pale and quickly return to its normal color (within 5 seconds).
- The dressing should be secure but not so tight that it cuts off circulation.
- Change Regularly:
- Replace dressings regularly to keep the wound clean, fresh, and dry.
- Watch for signs of infection like redness, pus, or fever, and seek medical help if they appear.
Bandaging Practical Class for Diploma In Pharmacy Course 1 Year
Bandaging is the process of applying strips of material to support, protect, compress, or immobilize a body part, often to hold a dressing over a wound, control bleeding, reduce swelling, or secure a splint, requiring clean technique and proper tension for effective healing and to prevent harm. Key principles involve using layers (primary, secondary, tertiary) and specific techniques like figure-8 wraps to ensure comfort, circulation, and proper wound care.
Key Purposes of Bandaging
- Wound Care: Holding dressings, absorbing exudate, protecting from infection, and creating a healing environment.
- Support: Immobilizing injuries like sprains or securing splints.
- Compression: Reducing soft tissue swelling and controlling bleeding.
- Medication Delivery: Some bandages can hold topical medications.
Basic Steps & Principles
- Prepare the Wound: Gently clean the wound with mild soap and water, rinse, and pat dry.
- Apply Dressing: Place a sterile dressing directly on the wound.
- Layering (for complex wounds):
- Primary: Direct contact with wound/dressing (e.g., gauze).
- Secondary: Provides absorption & stabilization (e.g., padding).
- Tertiary: Outer layer holding it all (e.g., roller bandage).
- Technique Matters: Use even tension, overlapping by half with each turn; avoid wrinkles.
- Check Circulation: Ensure the bandage isn’t too tight by checking for numbness, tingling, or color changes.
Common Bandage Types & Uses
- Roller Gauze: Versatile for securing dressings or light support.
- Elastic Bandages (Ace): For compression on sprains or to hold splints.
- Figure 8: Ideal for joints like ankles or elbows to allow movement while providing support.
Watch For
- Signs of Infection: Redness, swelling, pus, and increased pain.
- Circulatory Issues: Coldness, numbness, or bluish skin below the bandage.
Some Subjects Details Diploma In Pharmacy Course 1 Year Given Below
Human Anatomy and Physiology Diploma In Pharmacy Course 1 Year
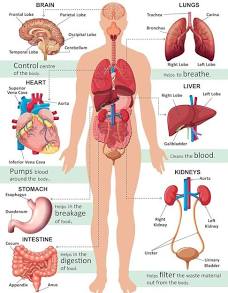
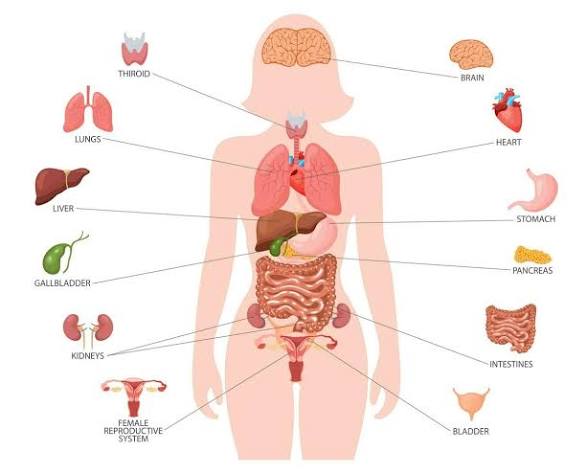
Human anatomy is the scientific study of the structures within the human body, divided into gross anatomy (visible to the naked eye) and microscopic anatomy (cells and tissues, studied with microscopes), crucial for medicine and understanding function, using dissection and modern imaging like MRI/CT scans to explore systems like skeletal, nervous, circulatory, and digestive.
Key Branches
- Gross Anatomy: Study of structures visible without magnification (e.g., organs, bones, muscles).
- Microscopic Anatomy: Study of minute structures, including:
- Histology: Tissues.
- Cytology: Cells.
- Regional Anatomy: Focuses on specific body regions (e.g., head, thorax).
- Systemic Anatomy: Focuses on organ systems (e.g., nervous, cardiovascular).
Major Body Systems (Examples)
- Skeletal System: Bones, providing structure and support.
- Muscular System: Muscles for movement.
- Circulatory System: Heart, blood vessels, blood (transport).
- Nervous System: Brain, spinal cord, nerves (control).
- Digestive System: Stomach, intestines, etc. (nutrient processing).
- Respiratory System: Lungs, airways (gas exchange).
- Integumentary System: Skin, hair, nails (protection).
Human Physiology:
Human physiology is the scientific study of how the human body’s cells, tissues, organs, and systems work and interact, from molecular mechanisms to organ-level functions, all aimed at maintaining a stable internal environment (homeostasis) through complex physical and biochemical processes to support life. It explains the “how” and “why” of normal bodily functions, like breathing, digestion, and movement, forming the foundation of medicine by showing how the body responds to health, stress, and disease.
Core Concepts
- Homeostasis: The body’s ability to maintain stable internal conditions (e.g., temperature, pH, blood sugar) despite external changes, a central theme in physiology.
- Levels of Organization: It examines functions from the smallest (molecules, cells) to the largest (organ systems, the whole organism).
- Interconnected Systems: Focuses on how systems like the nervous, endocrine, cardiovascular, and respiratory systems work together.
Key Areas of Study
- Cellular Physiology: How individual cells perform basic functions like energy production and reproduction.
- Organ System Physiology: How systems like the digestive, urinary, and circulatory systems carry out complex tasks.
- Exercise Physiology: How the body adapts to physical activity.
- Neurophysiology: How the nervous system transmits signals.

Major Systems of the Human Body
| System | Main Function |
|---|---|
| Skeletal | Support & protection |
| Muscular | Movement |
| Nervous | Control & coordination |
| Endocrine | Hormonal regulation |
| Cardiovascular | Blood circulation |
| Respiratory | Gas exchange |
| Digestive | Nutrition & digestion |
| Urinary | Waste excretion |
| Reproductive | Reproduction |
| Integumentary | Protection & temperature control |
Relationship Between Anatomy & Physiology
| Anatomy | Physiology |
|---|---|
| Structure | Function |
| Form | Action |
| Static study | Dynamic study |
কয়েকটি সিস্টেম সম্পর্কে আলোচনা করা হলো:
1. Skeletal System
Function:
- Gives shape and support to the body
- Protects vital organs (brain, heart, lungs)
- Helps in body movement
- Produces blood cells in bone marrow
Main Parts:
- Bones (206 bones)
- Joints
- Cartilage
2. Muscular System
Function:
- Enables movement of the body
- Maintains posture
- Produces heat
Types of Muscles:
- Skeletal muscle – voluntary
- Smooth muscle – involuntary
- Cardiac muscle – found in the heart
3. Nervous System
Function:
- Controls and coordinates body activities
- Receives and responds to stimuli
- Responsible for thinking, memory, and emotions
Main Parts:
- Brain
- Spinal cord
- Nerves
4. Cardiovascular System
Function:
- Circulates blood throughout the body
- Transports oxygen, nutrients, and hormones
- Removes waste products
Main Parts:
- Heart
- Blood
- Blood vessels (arteries, veins, capillaries)
5. Respiratory System
Function:
- Helps in breathing
- Supplies oxygen to the blood
- Removes carbon dioxide from the body
Main Parts:
- Nose
- Trachea
- Lungs
- Alveoli
6. Digestive System
Function:
- Digestion of food
- Absorption of nutrients
- Elimination of waste
Main Parts:
- Mouth
- Esophagus
- Stomach
- Intestines
- Liver and pancreas
Pharmacology-1 for Diploma In Pharmacy Course 1 Year
1. Definition of Pharmacology
Pharmacology is the branch of medical science that deals with drugs, their sources, actions, uses, side effects, and mechanisms in the human body.
2. Drug – Definition
A drug is a chemical substance that is used to diagnose, prevent, treat, or cure disease.
3. Branches of Pharmacology
- Pharmacokinetics – What the body does to the drug
- Pharmacodynamics – What the drug does to the body
- Pharmacotherapeutics – Use of drugs in treatment
- Toxicology – Study of harmful effects of drugs
- Chemotherapy – Drugs used to treat infections and cancer
4. Pharmacokinetics (ADME)
A – Absorption:
How a drug enters the bloodstream
D – Distribution:
How the drug spreads in the body
M – Metabolism:
Breakdown of drugs mainly in the liver
E – Excretion:
Removal of drugs mainly through kidneys (urine)
5. Pharmacodynamics
- Drug action and effect
- Receptor interaction
- Dose–response relationship
Example:
Paracetamol reduces pain and fever.
6. Routes of Drug Administration
- Oral (by mouth)
- Sublingual
- Intravenous (IV)
- Intramuscular (IM)
- Subcutaneous (SC)
- Topical
- Inhalation
7. Types of Drugs
- Analgesics (pain killers)
- Antibiotics
- Antipyretics (reduce fever)
- Antiseptics
- Sedatives
8. Adverse Drug Reactions (ADR)
- Nausea
- Vomiting
- Allergy
- Drowsiness
9. Importance of Pharmacology for Nurses / Physiotherapists
- Safe drug administration
- Understanding drug effects
- Prevention of medication errors
- Patient education
10. Common Terms
- Dose: Amount of drug given
- Therapeutic effect: Desired effect
- Side effect: Unwanted effect
- Overdose: Excess amount of drug
Study of OTC for Diploma In Pharmacy Course 1 Year
OTC Drugs are important for all Medical Assistant Courses. These Drugs are Emergency and safe for the patients. The Study of OTC Drugs improves the quality of practice. Some OTC Drugs are Albendazole, Ascorbic Acid, Calcium, Multivitamins, Vitamin B Complex, Omeprazole, Oral Rehydration Salt, Salbutamol etc.
1. Definition of OTC Drugs
OTC (Over-the-Counter) drugs are medicines that can be purchased without a doctor’s prescription and are used for minor illnesses.
2. Common Uses of OTC Drugs
- Headache
- Fever
- Cold & cough
- Mild pain
- Acidity
- Minor skin problems
3. Classification of OTC Drugs
A. Analgesics & Antipyretics
Use: Pain and fever
- Paracetamol
- Ibuprofen
⚠️ Side effects: Liver damage (overdose), gastric irritation
B. Antacids
Use: Acidity, heartburn
- Aluminum hydroxide
- Magnesium hydroxide
⚠️ Side effects: Constipation, diarrhea
C. Antihistamines
Use: Allergy, cold, sneezing
- Cetirizine
- Loratadine
⚠️ Side effects: Drowsiness
D. Cough & Cold Preparations
Use: Cough, sore throat
- Dextromethorphan
- Guaifenesin
E. Laxatives
Use: Constipation
- Isabgol
- Bisacodyl
F. Antiseptics & Disinfectants
Use: Wound cleaning
- Povidone-iodine
- Chlorhexidine
4. Advantages of OTC Drugs
- Easily available
- Low cost
- Useful for minor ailments
- Saves time
5. Disadvantages / Risks
- Wrong drug use
- Overdose
- Drug interactions
- Masking of serious disease
First Aid for Diploma In Pharmacy Course 1 Year
First Aid is an important subject for Medical courses including Diplomas in Medicine & Surgery course. RMP Courses, LMAF Courses, Paramedical Courses, DMA Courses, DMS Courses, Nursing Courses, Dental Courses, Pathology Courses, Physiotherapy Courses, Caregiver courses etc. Here we discuss shock, Classification Shock, causes of Shock, Stages of Shock, Clinical Features of Shock, Hypovolemic Shock, Cardiogenic Shock, Neurogenic Shock, Traumatic Shock, Burn Shock, Electric Shock, Psychogenic Shock, Anaphylactic Shock, First Aid of Shock, First Aid of cut, First Aid of Snake Bite, First Aid of Accidental Injury etc.
1. Definition
First Aid is the immediate and temporary care given to an injured or suddenly ill person before professional medical help is available.
2. Aims of First Aid
- Preserve life
- Prevent further injury
- Promote recovery
3. Basic Principles of First Aid
- Stay calm and ensure scene safety
- Check Airway, Breathing, Circulation (ABC)
- Call for medical help if needed
- Do not move the patient unnecessarily
4. Common First Aid Situations
A. Bleeding
- Apply direct pressure
- Elevate the injured part
- Use a clean bandage
B. Burns
- Cool the burn with running water (10–20 minutes)
- Do not break blisters
- Cover with a clean cloth
C. Fracture
- Immobilize the affected area
- Use splints if available
- Do not try to straighten the bone
D. Fainting
- Lay the person flat
- Raise legs
- Loosen tight clothing
E. Choking
- Encourage coughing
- Perform abdominal thrusts (Heimlich maneuver) if needed
F. Shock
- Lay patient down
- Keep warm
- Do not give food or drink
5. First Aid Kit Contents
- Sterile gauze
- Bandages
- Antiseptic solution
- Scissors
- Gloves
- Cotton
- Pain reliever
6. Importance of First Aid
- Saves lives
- Reduces severity of injury
- Provides confidence in emergencies
Antimicrobial Drugs for Diploma In Pharmacy Course 1 Year
Antimicrobial drugs are agents that kill or stop the growth of microorganisms like bacteria, viruses, fungi, and parasites, including key types like antibiotics (for bacteria), antivirals, antifungals, and antiparasitics, used to treat infections by targeting unique microbial processes while sparing host cells (selective toxicity). They work by mechanisms such as disrupting cell walls (antibiotics) or inhibiting replication, and are crucial in human and animal medicine, though their overuse drives antimicrobial resistance.
Types & Targets
- Antibiotics: Target bacteria (e.g., penicillin, amoxicillin).
- Antivirals: Target viruses (e.g., acyclovir for herpes).
- Antifungals: Target fungi (e.g., ketoconazole).
- Antiparasitics: Target parasites, including protozoa (e.g., mefloquine for malaria) and helminths (e.g., niclosamide for tapeworms).
How They Work (Mechanisms)
- Bactericidal: Kill bacteria directly (e.g., by destroying cell walls).
- Bacteriostatic: Prevent bacteria from multiplying, allowing the immune system to clear the infection.
- Selective Toxicity: Drugs are designed to harm microbial cells without harming human cells, a key principle.
Classification by Spectrum
- Broad-spectrum: Effective against a wide range of bacteria.
- Narrow-spectrum: Effective against a limited range of specific bacteria.
Other Related Terms
- Antiseptics: Applied to skin to reduce infection risk (e.g., alcohol, hydrogen peroxide).
- Disinfectants: Used on non-living surfaces to kill microbes
Cardiovascular Drugs for Diploma In Pharmacy Course 1 Year
Cardiovascular drugs are medications that manage heart and blood vessel conditions, working in various ways like lowering blood pressure (ACE inhibitors, beta-blockers, calcium channel blockers), reducing cholesterol (statins), preventing clots (anticoagulants, antiplatelets), or improving heart function (diuretics, inotropes). They treat hypertension, angina, heart failure, arrhythmias, and high cholesterol, with common examples including statins (atorvastatin), blood pressure meds (lisinopril, metoprolol, amlodipine), and blood thinners (warfarin, apixaban).
Common Types & Functions:
- Antihypertensives (Blood Pressure):
- ACE Inhibitors & ARBs: Relax blood vessels (e.g., lisinopril, losartan).
- Beta-Blockers: Slow heart rate and lower blood pressure (e.g., metoprolol, atenolol).
- Calcium Channel Blockers: Relax blood vessels by blocking calcium (e.g., amlodipine, nifedipine).
- Lipid-Lowering Drugs (Cholesterol):
- Statins: Block cholesterol production (e.g., atorvastatin, simvastatin).
- Anticoagulants & Antiplatelets (Blood Thinners): Prevent blood clots (e.g., warfarin, rivaroxaban, aspirin).
- Diuretics (Water Pills): Remove excess fluid, reducing blood volume (e.g., furosemide, hydrochlorothiazide).
- Anti-Arrhythmics: Control irregular heartbeats.
- Nitrates: Relieve angina by dilating blood vessels (e.g., nitroglycerin).
How They Work:
- Relaxing Vessels: ACE inhibitors, ARBs, Calcium Channel Blockers, Nitrates.
- Slowing Heart: Beta-blockers.
- Reducing Cholesterol: Statins.
- Preventing Clots: Anticoagulants, Antiplatelets.
- Increasing Contraction Force (for heart failure): Cardiac glycosides (e.g., Digoxin).
General Chemistry for Medical Science for Diploma In Pharmacy Course 1 Year
General Chemistry for Medical Science focuses on fundamental chemical principles (atoms, bonding, reactions, solutions, acids/bases, electrochemistry) and introduces organic/biological chemistry, serving as a crucial foundation for understanding medicines, human body processes, pharmacology, and clinical practice for future healthcare professionals like doctors, nurses, and med techs. It bridges basic science with health applications, covering essential lab safety and skills for medical fields.
Key Topics Covered
- Basic Principles: Atomic structure, periodic table, stoichiometry, states of matter, thermodynamics, kinetics, equilibrium, solutions.
- Core Concepts: Acids & bases, electrochemistry, bonding, intermolecular forces.
- Biological Focus: Introduction to organic and biological chemistry, explaining chemical processes in living systems.
- Health Applications: Relevance to drugs, medical devices, and clinical settings, emphasizing safety (PPE, fire, radiation) and rationale for treatments.
Why It’s Important for Medical Science
- Foundation for Advanced Study: Prepares students for biochemistry, pharmacology, and clinical chemistry.
- Understanding Medications: Helps understand how drugs work, their interactions, and parameters (absorption, distribution, metabolism, excretion).
- Informed Healthcare: Leads to better-informed doctors, nurses, and other professionals in a scientifically advancing field.
- Medical School Prerequisites: Often required for entry into medical and allied health programs (Nursing, Med Tech).
Respiratory Drugs for Diploma In Pharmacy Course 1 Year
Respiratory drugs treat lung and airway issues like asthma, COPD, and infections by relaxing airways (bronchodilators like albuterol), reducing inflammation (corticosteroids), clearing mucus (expectorants/mucolytics), controlling allergies (antihistamines), and fighting bacteria (antibiotics), often delivered via inhalers for direct lung action. Key types include bronchodilators (beta-agonists, anticholinergics), anti-inflammatories, leukotriene modifiers, and combination inhalers for targeted relief and long-term control.
Types of Respiratory Drugs & Their Uses:
- Bronchodilators: Open airways, easier breathing.
- Beta-2 Agonists (SABA/LABA): Albuterol (short-acting), Salmeterol (long-acting) for asthma/COPD.
- Anticholinergics (SAMA/LAMA): Ipratropium, Tiotropium for COPD.
- Methylxanthines: Theophylline for severe asthma/COPD.
- Anti-inflammatories: Reduce swelling and mucus.
- Corticosteroids: Fluticasone, Prednisone (oral) for inflammation.
- Leukotriene Receptor Antagonists (LTRAs): Montelukast (not detailed in snippets, but a key type).
- Combination Inhalers: Mix bronchodilators and corticosteroids (e.g., LABA/ICS) for better control.
- Mucolytics/Expectorants: Thin mucus for easier coughing up (e.g., Ambroxol).
- Antihistamines & Decongestants: For allergy symptoms (runny nose, sneezing).
- Antibiotics: Treat bacterial infections (e.g., Amoxicillin, Doxycycline).
- Antitussives: Suppress coughs (e.g., Dextromethorphan – not in snippets but related).
Common Delivery Methods:
- Inhalers (MDI/DPI): Metered-dose inhalers or dry powder inhalers for direct lung delivery.
- Nebulizers: Turn liquid medicine into a mist.
- Oral: Tablets, syrups (e.g., oral steroids, theophylline).
How They Work:
- Relievers (Short-acting): Quick relief for sudden symptoms (e.g., SABA).
- Controllers/Preventers (Long-acting/Steroids): Daily use to prevent attacks and control underlying inflammation.
 HRTD Medical Institute HRTD Medical Institute
HRTD Medical Institute HRTD Medical Institute

